






InUrSkn is more than just a skin a hair and body clinic. It is Dr. Sejal's promise of providing minimal intervention patient care which is holistic, personalized and humane.












Fungal skin infections, caused by fungi invading the skin, can manifest as itching, scaling, or redness. Common types include athlete’s foot, ringworm, and jock itch. Treatment often involves antifungal creams, lotions, or oral medications. Keeping the affected area clean and dry, alongside prompt medical treatment, can effectively manage and cure the infection. It’s advisable to seek healthcare advice for an accurate diagnosis and tailored treatment plan to prevent recurrence or worsening of the infection.
Read More
Bacterial skin infections are common conditions caused by harmful bacteria, often presenting as redness, swelling, and tenderness. Prompt medical attention and hygiene practices are crucial for management. Treatment typically includes topical or oral antibiotics to combat the infection. It’s vital to follow dermatologists’ instructions, keeping the area clean and avoiding further irritation to promote healing. For recurring or severe infections, specialized medical care may be necessary to prevent complications and ensure effective treatment.
Read More
Viral skin infections, caused by viruses, manifest in various forms like warts or shingles. Their treatment and management largely depend on the specific virus involved. Over-the-counter topical treatments may alleviate symptoms, though severe cases require medical intervention. Antiviral medications prescribed by dermatologists can combat the virus, lessen symptoms, and expedite healing. Maintaining good hygiene and following a dermatologist’s advice is essential for managing viral skin infections and preventing their spread to others.
Read More
Parasitic skin infections result from infestations by organisms such as lice, scabies, or mites. They often cause intense itching, rashes, and discomfort. Effective treatment usually involves topical or oral medications to eradicate the parasites, prescribed by a dermatologist. Additionally, thorough cleaning of personal belongings and living environments is crucial to prevent re-infestation. Consultation with a dermatologist is vital for an accurate diagnosis and treatment plan, ensuring complete eradication of the parasites and relief from symptoms.
Read More
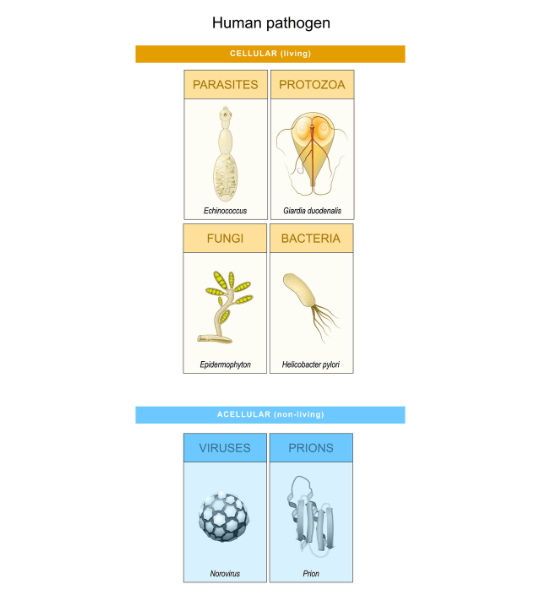
A skin infection occurs when harmful microorganisms such as bacteria, viruses, fungi, or parasites invade the skin and multiply, causing varying degrees of skin and tissue damage. These infections often manifest as redness, swelling, itching, rash, and sometimes the formation of pus or discharge.
There are various types of skin infections, each caused by different types of microorganisms:
1. Bacterial Skin Infections: These are often caused by strains of Staphylococcus and Streptococcus bacteria. Common bacterial infections include cellulitis, impetigo, and folliculitis. Treatment usually involves antibiotics.
2. Viral Skin Infections: Viral infections are caused by viruses, with common examples being warts, herpes simplex, and shingles. Treatment varies with the type of virus, but may include antiviral medications.
3. Fungal Skin Infections: Fungi cause infections like athlete’s foot, ringworm, and yeast infections. They thrive in warm, moist environments and can be treated with antifungal medications.
4. Parasitic Skin Infections: Parasites such as lice and mites cause infections like scabies. Treatment typically involves topical or oral medications to eliminate the parasites.
Prompt diagnosis and treatment are crucial to managing skin infections effectively, preventing further complications, and ensuring a complete recovery. It’s advisable to consult with a dermatologist who can provide an accurate diagnosis based on the type of infection and prescribe the appropriate treatment plan. Maintaining good personal hygiene, keeping the skin clean and dry, and avoiding contact with infected individuals can help prevent the occurrence of skin infections.

Fungal skin infections, caused by fungi invading the skin, can manifest as itching, scaling, or redness. Common types include athlete’s foot, ringworm, and jock itch. Treatment often involves antifungal creams, lotions, or oral medications. Keeping the affected area clean and dry, alongside prompt medical treatment, can effectively manage and cure the infection. It’s advisable to seek healthcare advice for an accurate diagnosis and tailored treatment plan to prevent recurrence or worsening of the infection.
Ringworm is the most common fungal infection. It presents as itchy red ring shaped lesions on groin, under arms and other folds. It can also occur on hands, feet, nails and scalp. It is contagious. Factors that aggravate ringworm are : Increased sweating, Humidity, Diabetes etc.
Ringworm can manifest on other parts of the body differently and has different names for the same. When it occurs on the foot it is called Athlete’s foot and when it occurs on the groin or thigh areas it is called jock itch.
Other common fungal infections of the skin include:
Pityriasis Versicolor : It is seen as multiple white spots or patches on face, upper chest, back and arms. Causes for the same include, hot humid conditions and sweating.
Candidiasis : It presents as red itchy rashes on the groin, under arms, genital areas. It is associated with diabetes.
Onychomycosis is a fungal infection of your nails. It can affect the fingernails or the toenails, although infections of the toenails are more common.
Things that can cause or aggravate fungal infections are:
Living in a warm or wet environment
Sweating heavily
Not keeping your skin clean and dry
Sharing items like clothing, shoes, towels, or bedding
Wearing tight clothing or footwear that doesn’t breathe well
Taking part in activities that involve frequent skin-to-skin contact
Coming into contact with animals that may be infected
Having a weakened immune system due to immunosuppressant drugs, cancer treatment, or conditions such as HIV
Be sure to practice good hygiene.
Don’t share clothing, towels, or other personal items.
Wear clean clothes every day, particularly socks and underwear.
Choose clothing and shoes that breathe well. Avoid clothing or shoes that are too tight or have a restrictive fit.
Make sure to dry off properly with a clean, dry, towel after showering, bathing, or swimming.
Wear sandals or flip-flops in locker rooms instead of walking with bare feet.
Wipe down shared surfaces, such as gym equipment or mats.
Stay away from animals that have signs of a fungal infection, such as missing fur or frequent scratching.
Antifungal medications are available in oral and topical forms. Topical antifungals prescribed maybe in the powder, ointment, cream or spray forms.
Fungal skin infections are caused by the overgrowth of fungi on or in the skin, which can result from factors like a warm, moist environment, sweating, poor hygiene, or a weakened immune system.
Yes, many fungal skin infections are contagious and can be spread through direct skin-to-skin contact or indirectly through contaminated objects, clothing, or surfaces.
Diagnosis is usually done by a dermatologist based on the appearance of the skin and may be confirmed through skin scrapings, cultures or a biopsy to examine the fungus under a microscope or grow it in a laboratory.
The duration of a fungal skin infection varies depending on the type of infection, the area affected, and the effectiveness of treatment. With appropriate treatment, some infections may clear up in a few weeks, while others may take longer.
While typically not dangerous, they can cause discomfort and cosmetic concerns. However, in individuals with weakened immune systems, fungal infections could potentially lead to more serious complications.
Yes, fungal skin infections can recur, especially if the underlying conditions that favor fungal growth are not addressed.
Prevention strategies include maintaining good hygiene, keeping the skin dry, avoiding sharing personal items, wearing breathable clothing, and staying away from individuals or animals with visible fungal infections.
Over-the-counter antifungal creams may be effective for mild fungal skin infections, but more severe or persistent infections may require prescription-strength antifungal medications.
Some natural remedies like tea tree oil or coconut oil are believed to have antifungal properties, but their effectiveness can vary and they may not be a substitute for medical treatment. It’s advisable to consult with a dermatologist before trying natural remedies.
A balanced diet that supports a strong immune system may help in preventing or managing fungal skin infections. Additionally, reducing sugar intake might be beneficial as fungi like Candida thrive on sugar.
If you suspect you have a fungal skin infection, if over-the-counter treatments have not worked, or if the infection is spreading, it’s advisable to see a dermatologist for a proper diagnosis and treatment plan.
It’s best to avoid activities that cause excessive sweating or skin-to-skin contact until the infection is treated. Ensure the affected area is covered to avoid spreading the infection.
While uncommon, severe or untreated fungal infections might lead to secondary bacterial infections or other complications, especially in individuals with weakened immune systems.
Steroid creams can alleviate itching and inflammation but do not treat the fungal infection. They can sometimes worsen the infection. It’s advisable to consult a dermatologist before using steroid creams on fungal infections.
Fungal and bacterial infections are caused by different microorganisms and often have different symptoms, appearances, and treatments. A dermatologist can accurately diagnose the type of infection and prescribe the appropriate treatment.

Bacterial skin infections are common conditions caused by harmful bacteria, often presenting as redness, swelling, and tenderness. Prompt medical attention and hygiene practices are crucial for management. Treatment typically includes topical or oral antibiotics to combat the infection. It’s vital to follow dermatologists’ instructions, keeping the area clean and avoiding further irritation to promote healing. For recurring or severe infections, specialized medical care may be necessary to prevent complications and ensure effective treatment.
Some of the common bacterial skin infections include:
Cellulitis affects the two deepest layers of the skin—the dermis and the subcutaneous tissue. It often appears as a swollen, red area on the skin and feels tender and hot when touched.
Erysipelas infects the top two layers of the skin. It is commonly known as “St. Anthony’s Fire” because of the intense, burning sensation that occurs with it. Symptoms include extreme redness, swelling, and a sharply defined border between the normal and infected skin. It is similar in appearance to cellulitis.
Bacterial folliculitis is a relatively common infection of the hair follicles. It is usually caused by a fungus, ingrown hair, or blockages from moisturizers or other products applied to the skin. Shaving or plucking hairs can also increase risk. Symptoms of bacterial folliculitis include tiny, red bumps or white-headed pimples filled with pus. This infection tends to occur more often in people with acne than those who have clearer skin.
Hot tub folliculitis causes pus-filled bumps and an itchy red rash. These symptoms come on a few hours to several days after exposure to the bacteria that cause it. It is sometimes called “Pseudomonas folliculitis” or “Jacuzzi folliculitis” because it is contracted through contaminated whirlpools and hot tubs
A furuncle, more commonly known as a boil, is a painful infection around a hair follicle. It begins as a red lump, which may be tender, and rapidly fills with pus as it gets bigger. If left untreated, a furuncle can develop into an abscess.
Impetigo is a bacterial infection of the top layer of epidermal skin. It is highly contagious and more commonly seen in children than adults.8 Caused by Streptococcus and Staphylococcus, the impetigo rash is covered by a honey-colored crust.
Erythrasma is a superficial skin infection caused by the Corynebacterium minutissimum bacteria. At the beginning, symptoms include well-defined pink patches of skin covered with fine scales and wrinkling. The rash becomes red, then brown and scaly.
Methicillin-resistant Staphylococcus aureus (MRSA) is a serious bacterial infection that is resistant to standard antibiotic treatment. It will often cause a mild, blister-like sore on the skin.
Wash your hands often and properly.
Wash scrapes, cuts, wounds, or insect bites right away.
Do not share items, such as towels, razors, bar soap, clothes, or toys.
Avoid skin-to-skin contact with anyone who has a skin infection.
Cover any skin infections with a bandage after skin is clean and dry.
Clean any shared toys, bedding, or changing tables.
Bacterial skin infections are treated with topical and oral antibiotics. In rare conditions antibiotic injections or drips may also be needed.
Symptoms may include redness, swelling, tenderness, warmth in the affected area, and sometimes fever or drainage of pus. A dermatologist can provide an accurate diagnosis.
Yes, if left untreated, the bacteria can spread to other areas of your body or to other people. It’s crucial to get prompt treatment and follow hygiene practices to prevent spread.
Treatment usually involves topical or oral antibiotics. The specific treatment may vary depending on the type and severity of the infection.
It may take a few days to a few weeks for the infection to clear, depending on its type and severity. It’s important to complete the full course of prescribed antibiotics to ensure the infection is fully eradicated.
Yes, bacterial skin infections can recur, especially if the underlying cause or contributing factors aren’t addressed.
Yes, severe or improperly treated bacterial infections can cause scarring. Early treatment and following your dermatologist’s instructions can minimize the risk of scarring.
Keep your skin clean, treat wounds promptly, avoid contact with others’ wounds or bandages, and avoid skin-to-skin contact with individuals who have a skin infection.
It’s essential to see a dermatologist for a proper diagnosis and treatment plan. Home remedies may not be effective and could potentially worsen the infection.
Untreated or severe bacterial skin infections can lead to deeper infections, sepsis, or other serious health issues, particularly in individuals with weakened immune systems.
The symptoms, appearance, and the affected area can be different, but a precise diagnosis should be made by a dermatologist through physical examination and possibly culture tests.
Over-the-counter antibiotic ointments may help for very minor infections, but it’s always best to consult with a dermatologist for the appropriate treatment plan.
If you suspect a bacterial skin infection, have persistent or worsening symptoms, or if over-the-counter treatments are ineffective, you should see a dermatologist promptly.
It’s advisable to avoid exercising until the infection has been treated, to prevent spreading the bacteria through sweat or contact with gym surfaces or equipment.
Covering the infection with a clean, dry bandage can help prevent the spread of bacteria. Change the bandage as directed by your dermatologist.
Yes, warm and humid climates can promote bacterial growth and increase the likelihood of bacterial skin infections. Keeping the skin clean and dry can help mitigate this risk.

Viral skin infections, caused by viruses, manifest in various forms like warts or shingles. Their treatment and management largely depend on the specific virus involved. Over-the-counter topical treatments may alleviate symptoms, though severe cases require medical intervention. Antiviral medications prescribed by dermatologists can combat the virus, lessen symptoms, and expedite healing. Maintaining good hygiene and following a dermatologist’s advice is essential for managing viral skin infections and preventing their spread to others.
The most common viral skin infections include:
Chickenpox is a viral infection. It presents as red blisters which are itchy painful with a burning sensation seen on face, chest, back and is often accompanied by fever. Complications like pneumonia, meningitis may be seen more commonly in adults.
Herpes is a viral infection, contagious in nature. Spreads by close contact with infected person. It presents as burning and painful water filled blisters which on rupture forms crust. It is sometimes associated with fever. It is commonly seen on lips, inside of mouth, fingers, eyes. Infection is known to recur when immunity is low.
Herpes zoster is also known as shingles. It is caused by reactivation of chickenpox virus. It is commonly seen after 40 years of age. It Presents as painful blisters occurring on one side of the body followed by crusting. Scarring is more common seen in elderly patients. Pain occurs in the area supplied by the affected nerve. Sometimes pain can last longer
Hand Foot Mouth (HFM) disease is a viral infection which is contagious by nature. It is commonly seen in children, but can also be seen in adults. It presents as multiple water filled painful blisters seen on hands, feet, buttocks, elbows and mouth. HFM is associated with fever. Typical healing begins in 4 to 5 days.
Molluscum contagiosum is a skin infection caused by a virus of the same name. It produces benign, raised bumps, or lesions, on the upper layers of your skin. The small bumps are usually painless. They resolve without treatment and rarely leave scars. The length of time the virus lasts varies for each person, but the bumps can remain from 2 months to 4 years.
Warts are raised bumps on your skin caused by the human papillomavirus (HPV). Although warts generally aren’t dangerous, they can be uncomfortable, potentially embarrassing, and contagious. They can also be painful.
Measles, or rubeola, is a viral infection that starts in the respiratory system. It still remains a significant cause of death worldwide, despite the availability of a safe, effective vaccine. A widespread skin rash is a classic sign of measles. This rash can last up to 7 days and generally appears within 14 days of exposure to the virus. It commonly develops on the head and slowly spreads to other parts of the body.
Since the mode of transmission of viruses can vary, it follows that one must keep not just physical contact hygiene in mind but also respiratory hygiene.
Some viral infections have antiviral drugs which have very good efficacy against the causative virus other conditions may not have an appropriate antiviral available. In such cases most of the treatment is around the symptoms.
A dermatologist may diagnose viral skin infections through a physical examination, medical history, and sometimes, laboratory tests such as skin biopsies or cultures.
Some viral skin infections can be cured, while others, like herpes, remain in the body and can cause recurrent outbreaks. Early medical intervention can help manage symptoms and prevent complications.
The duration varies depending on the virus and individual health conditions. Some infections resolve within days, while others may persist for weeks or longer, or cause recurrent outbreaks.
Many viral skin infections, like herpes or warts, are highly contagious. Following hygiene practices and avoiding skin-to-skin contact with infected individuals can help prevent transmission.
It depends on the virus. Some viruses, like chickenpox, usually provide immunity after infection, while others, like herpes, can cause recurrent outbreaks.
Yes, some viral skin infections can lead to other complications like bacterial infections, skin discoloration, or scars. Severe viral infections may affect other body systems as well.
Individuals with weakened immune systems, such as those with HIV/AIDS or undergoing cancer treatment, may be more susceptible to viral skin infections.
Yes, vaccinations can prevent certain viral skin infections like chickenpox, shingles, and measles. It’s advisable to stay updated on recommended vaccinations.
While there are some over-the-counter treatments available, their effectiveness may vary. It’s advisable to consult a dermatologist for appropriate treatment recommendations.
Maintaining a healthy diet can support your immune system, which may help prevent or manage viral skin infections. Discuss any dietary concerns with your dermatologist.
Avoid scratching or picking at lesions, keep the area clean, and follow your dermatologist’s treatment recommendations to minimize scarring.
Yes, some viral skin infections may affect specific areas, like warts on the hands or feet. Others may have a more widespread impact on the body.
Maintain good hygiene, cover the affected area, avoid sharing personal items, and avoid skin-to-skin contact with others to minimize spreading the infection.
It’s advisable to avoid public places, especially if the infection is in an active or contagious stage, to prevent spreading it to others.
Yes, there are many different types of viral skin infections, each caused by different viruses and presenting with varying symptoms and severities.
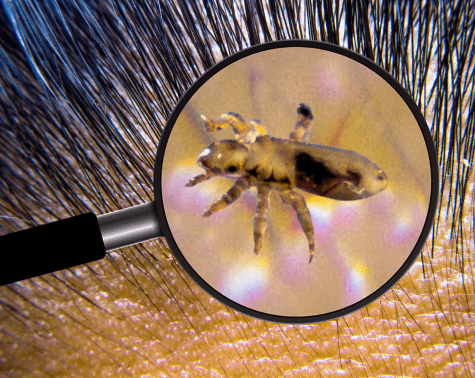
Parasitic skin infections result from infestations by organisms such as lice, scabies, or mites. They often cause intense itching, rashes, and discomfort. Effective treatment usually involves topical or oral medications to eradicate the parasites, prescribed by a dermatologist. Additionally, thorough cleaning of personal belongings and living environments is crucial to prevent re-infestation. Consultation with a dermatologist is vital for an accurate diagnosis and treatment plan, ensuring complete eradication of the parasites and relief from symptoms.
Scabies is caused by scabies mite. It is seen as tiny blisters in finger web spaces, abdomen, under arms and genital areas. Scabies is accompanied by intense itching. It is a highly contagious disease. Effects like itching may persist beyond two months after treatment also.
Head Lice are small, wingless, blood-sucking insects. They live in the hair on your head and feed off the blood from your scalp. These cause extreme scalp itchiness, feeling like something is crawling on your scalp and sores & scabs on your scalp from scratching.
Cutaneous larva migrans (CLM) is an infectious syndrome caused by multiple types of hookworms. This is most commonly transmitted by contact with animal feces and soil. The parasites lay eggs in the feces which is mixed with the soil. The eggs hatch and the larvae enter humans through direct contact with skin.
Hygiene aspects must be considered for prevention of such conditions. As an example Scabies is prevented by avoiding direct skin-to-skin contact with an infected person or with items such as clothing or bedding used by an infected person. For preventing head lice, one must avoid head to head contact and sharing objects of daily use like towels and combs.
The treatment for parasitic infections is generally based on killing the mites and their eggs. Sometimes physical extraction may also be needed.
A dermatologist may diagnose parasitic skin infections through a physical examination, medical history, and sometimes, laboratory tests such as skin scrapings or biopsies.
Yes, with appropriate treatment, parasitic skin infections can usually be cured. It’s crucial to follow the treatment plan provided by a dermatologist to ensure complete eradication of the parasites.
The duration of infection can vary depending on the type of parasite and the effectiveness of treatment. Early diagnosis and treatment can shorten the duration of the infection.
Many parasitic skin infections, such as scabies and lice, are highly contagious. It’s advisable to avoid close contact and sharing personal items with others while infected.
Yes, re-infestation can occur if you come into contact with the parasite again or if the initial treatment wasn’t effective in eradicating the parasites completely.
Yes, complications such as secondary bacterial infections or severe skin inflammation can occur, particularly if the skin is scratched and becomes broken.
Individuals with weakened immune systems or those living in crowded conditions may be at higher risk for parasitic skin infections. Travel to endemic areas may also increase risk.
Prevention measures include practicing good hygiene, avoiding contact with infected individuals, and thorough cleaning of personal belongings and living environments.
Treatments include topical or oral medications to eradicate the parasites. Additionally, physical extraction of larger parasites may be necessary in some cases.
While some home remedies are suggested online, it’s crucial to consult with a dermatologist before attempting any treatment to ensure it’s safe and effective.
Scratching the affected area can lead to wounds and potential scarring. Following the treatment plan and avoiding scratching can help minimize this risk.
Usually, with appropriate treatment, parasitic skin infections don’t cause long-term damage. However, severe infections or complications could potentially lead to lasting issues.
Avoiding close contact, sharing personal items, and following a diligent cleaning routine for your belongings and environment can help prevent the spread of infection.
It’s advisable to avoid public places until you have received treatment and are no longer contagious to prevent spreading the infection to others.
Yes, some parasitic skin infections can spread to other areas of the body if left untreated. Following your treatment plan diligently can help prevent this.


MD, DNB - Dermatology & Venereology
Dr. Sejal has dual degrees of MD and DNB in Dermatology and Venereology. She has worked with some of the senior most doctors in the largest government and private hospitals for more than 15 years. Over these years at InUrSKn, she has treated thousands of patients for a variety of conditions and needs across dermatology, venereology, cosmetology and trichology domains.
Dr. Sejal believes in a minimum intervention approach to health and believes that educating and empowering the patient is the key to good health.
Every patient at InUrSkn is seen personally by Dr. Sejal without any time limit, where she discusses the patient’s concern in detail along with understanding the history of their health and carrying out a personal examination.

At InUrSkn, we believe that all patient care must be:
– Holistic
– Personalized
– Humane
– Minimal
Dr. Sejal and her team live by the philosophy of never prescribing medications or procedures that may not be required. When addressing a concern, Dr. Sejal ensures that a detailed history and context are thoroughly understood. Medical tests are prescribed by Dr. Sejal only when she believes there is more to the concern that needs to be addressed, ensuring the patient truly benefits.
Multiple spacious procedure rooms
Full-fledged operation theatre
In-house laboratory
Latest technology
100+ Skin, Hair & Body Procedures offered
Frequent disinfection of all clinic spaces with UVC light and WHO-approved chemicals
Large waiting and treatment areas to ensure social distancing
Regular health checks for all patients and staff
Safer than salons, chain-clinics & hospitals
PPEs for patients and staff
Personal attention from Dr. Sejal Saheta (MD, DNB) - with 15+ years of experience
CIDESCO-certified aestheticians with minimum 3 years work experience
500+ Positive Reviews on Practo and Google
5000+ Patients treated last year alone
8000+ Procedures completed
| Prices | ||
|---|---|---|
| Procedure | ||
| In Clinic Consultation with Dr. Sejal | ||
| In Clinic Consultation with Dr. Sejal | ₹1100 | |
| Online Consultation with Dr. Sejal | ||
| Online Consultation with Dr. Sejal | ₹900 | |
Pricing (Inclusive of taxes)


Symptoms may include redness, swelling, itching, discomfort, blisters, and sometimes, discharge from the affected area.
Diagnosis often involves a physical examination, medical history review, and possibly laboratory tests such as cultures or skin biopsies, conducted by a dermatologist.
Factors may include a weakened immune system, poor hygiene, close contact with infected individuals or animals, or pre-existing skin conditions.
Practicing good hygiene, avoiding contact with infected individuals, and keeping wounds clean and covered can help prevent the spread of skin infections.
Treatment may include topical or oral medications, antiseptics, and in some cases, surgical intervention to drain abscesses. The exact treatment depends on the type and severity of the infection.
Over-the-counter treatments may be available for minor skin infections, but it’s advisable to consult with a dermatologist for an accurate diagnosis and treatment plan.
The duration can vary widely based on the type of infection and the effectiveness of the treatment. Some may resolve in a few days, while others could last several weeks or longer.
Many skin infections are contagious, but the degree of contagion depends on the type of infection and how it’s transmitted.
Yes, certain skin infections can recur, especially if the underlying cause is not effectively treated or the individual is re-exposed to the infectious agent.
Keeping the skin clean and dry, maintaining a healthy lifestyle to support immune function, and avoiding contact with known infectious agents can minimize risk.
If you suspect you have a skin infection, it’s wise to see a dermatologist promptly, especially if the infection is spreading, painful, or accompanied by fever.
Yes, some skin infections can cause scarring, especially if they’re severe or if the skin is scratched or otherwise irritated.
Over-the-counter creams and lotions may provide temporary relief, but a dermatologist can provide tailored advice based on your specific condition.
It may be advisable to keep a skin infection covered to prevent spreading the infection to other parts of the body, but it’s best to follow the guidance of a dermatologist.
Some vaccinations can prevent certain types of viral skin infections, like chickenpox and shingles. Consult with a dermatologist for personalized advice.


Ready to book an appointment?
BOOK

Want to talk about your needs ?
MAKE AN enquiry
