






InUrSkn is more than just a skin a hair and body clinic. It is Dr. Sejal's promise of providing minimal intervention patient care which is holistic, personalized and humane.













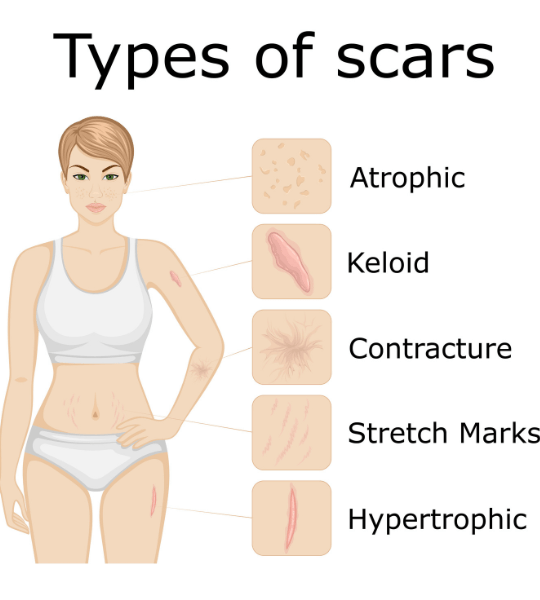
Depressed (Atrophic) Scars manifest when there’s an inadequate regeneration of skin tissue post-injury, resulting in an indented appearance unlike the raised texture of keloid or hypertrophic scars. Commonly linked to chickenpox, acne, or mole removal, these scars indicate healing below the normal skin level. Three variants exist: icepick scars with a deep pore appearance, boxcar scars resembling chickenpox scars, and rolling scars, distinguished by undulating edges, commonly found on cheeks.
Read More
Contracture scars usually form post-burn, leading to skin tightening, thus hampering mobility especially when extending to muscles, nerves, or over joints. Treatment is challenging, commonly requiring surgical procedures to alleviate the contracted area and regraft skin. Such scars notably affect not only the physical aspect but also one’s quality of life, necessitating early and effective intervention for better rehabilitation and function.
Read More
Keloidal scars, unlike the initially flat scars, tend to enlarge progressively and don’t flatten over time. They extend beyond the wound site, often appearing raised, red or dark, and can be itchy or painful. Treatment might include surgical removal, steroid injections, or laser therapy, although recurrence post-treatment is common. They can be aesthetically concerning and potentially hinder movement depending on the location.
Read More
Raised (Hypertrophic) scars, unlike keloidal scars, remain confined to the original wound area and typically develop post-injury or surgery. They rise above the skin’s surface due to excess collagen production during healing, but don’t extend beyond the wound boundary. Though less itchy and not as prone to continuous growth, they can be red and unsightly. Treatment options like silicone sheets, steroid injections, or laser therapy can help in flattening and improving the scar appearance.
Read More
Flat scars are initially slightly raised but flatten over time, transitioning from a pink or red color to a darker tone. They are considerably manageable and can be treated effectively with skin resurfacing procedures. For associated hyperpigmentation, treatments targeting melanin formation, such as Q-switched lasers, are employed to mitigate the darkened appearance, aiding in achieving a more even skin tone and smoother texture.
Read More
When you injure your skin, the body reacts to it by initiating an inflammation response to the injury which first contains the injury and then starts the tissue repair process. During the tissue repair phase there is a proliferation of cells from the adjoining areas to the injured area and the wound is closed with the formation of collagen and elastin fibres. (Collagen is a protein which is one of the basic building blocks of all tissue, skin, bones, etc.)
However as the skin and tissue heal, often the healed area becomes uneven and has a different texture and quality because of the nature of the injury. And hence we get what is called as scar tissue.
When a scar first develops on lighter skin, it’s usually pink or red. Over time, the pinkish colour fades, and the scar becomes slightly darker or lighter than the colour of the skin. In people with dark skin, scars often appear as dark spots.
The appearance of a scar depends on several factors such as:
– Injury or event that caused the scar, such as surgery, a burn or severe acne.
– Size, severity and location of the wound.
– Treatment you received for the wound, such as stitches or bandages.
– Your age, genes, ethnicity and overall health.

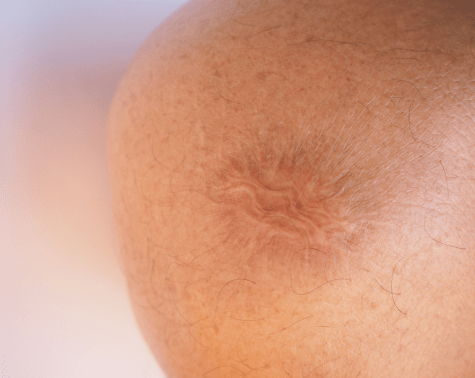
An atrophic scar develops when the skin cannot regenerate tissue correctly. Unlike keloids and hypertrophic scars, atrophic scars are indented in appearance due to healing that occurs below the expected layer of skin. This type of scar is most commonly associated with chickenpox or acne, although they also form as the result of having a mole removed .
There are three distinct types of atrophic scar. Atrophic scars that have the appearance of a deep pore are known as icepick scars. Flat-bottomed scars that resemble chickenpox scars are defined as boxcar scars. Finally, rolling scars are identified by a lack of distinct edges and are typically located around the cheeks.
Some atrophic scars may fade slightly over time, but they generally remain visible without treatment.
Yes, individuals with certain genetic predispositions or those with severe cases of acne or chickenpox may be more prone to developing atrophic scars.
Yes, dermal fillers can temporarily improve the appearance of atrophic scars by elevating the depressed skin.
Prompt treatment of acne, avoiding picking or squeezing of spots, and keeping wounds clean and covered can help in reducing the likelihood of atrophic scar formation.
Yes, cosmetic products like concealer or foundation can be used to temporarily cover atrophic scars, although they won’t improve the actual scarring.
Atrophic scars are characterized by a sunken appearance, whereas hypertrophic scars and keloids are raised above the skin’s surface.
Yes, microneedling can stimulate collagen production and improve the appearance of atrophic scars over multiple sessions.
Subcision is a surgical procedure that involves breaking the fibrous strands anchoring the scar to the underlying tissue, helping to elevate the depressed scar.
Often developing after a burn, a contracture scar causes the skin to tighten (contract). These scars can make it difficult to move, especially when the scarring gets into the muscles and nerves or occurs over a joint.
These are the most difficult types of scars to treat and generally need surgical intervention to relieve the contracture area and regrafting of skin into the affected area.
They predominantly develop following severe burns, leading to skin tightening due to the body’s healing process.
Unlike others, they restrict movement, possibly affecting muscles, nerves, and can be particularly challenging over joints.
They are relatively permanent but treatments like surgery can help improve mobility and appearance.
Procedures include scar release surgery, skin grafts, and sometimes tissue expansion to improve flexibility and appearance.
Yes, physiotherapy can help improve the range of motion and strengthen the surrounding muscles.
Immediate and appropriate burn wound care, early physiotherapy, and wearing pressure garments can help in prevention.
Yes, there’s a possibility especially if post-operative care and recommended physical therapy aren’t adhered to.
They can significantly impair mobility, causing difficulty in daily tasks and can be aesthetically displeasing.
Yes, treatments like laser therapy, and steroid injections may offer some relief, although results may vary.
Yes, they can potentially cause additional complications like joint deformities or neuropathic pain.

Some people have a tendency to developing keloidal scars. These scars are raised above the skin’s surface and spread beyond the wounded area. These are slightly itchy. The overgrown scar tissue can get large and may affect movement. Commonly seen on the chest or any surgical scars or deep injury.
Keloid scars are often treated with varied methods like:
-Excision using surgical blades or lasers.
– Intralesional Steroid Injections (ILS Injections)
However they have a high chance of recurrence. Some individuals are more likely to generate keloids. Also keloids can be familial in nature.
They result from an overproduction of collagen during wound healing, often related to an individual’s genetic predisposition.
Unlike hypertrophic scars which remain within the wound boundaries, keloids expand beyond the original wound area.
While non-cancerous, they might cause discomfort, itching, or pain, and can potentially impede movement in severe cases.
Areas with little fatty tissue like chest, back, shoulders, and ears are more prone to keloidal scarring.
Treatments include steroid injections, laser therapy, cryotherapy, surgical removal, or radiation therapy.
Yes, there’s a high recurrence rate post-treatment, sometimes growing larger than the original keloid.
Prompt and proper wound care, pressure therapy, or silicone gel sheeting can help in reducing the likelihood of keloids.
Laser treatment can help in reducing redness and improving texture, although may not eliminate the keloid entirely.
In rare instances, they can ulcerate or get infected, necessitating medical attention.
They might diminish in appearance over many years but generally do not disappear completely without treatment.

You can feel a hypertrophic scar when you run your finger over it. These raised scars may get smaller over time, but they never completely flatten out. Unlike keloids, they don’t grow or spread beyond the wounded area.
A major difference between raised scars and keloids is the fact that in keloids have extremely thick bands of connective tissue in the inner layers which do not allow for an easy resolution.
Overproduction of collagen during the healing process post-injury or surgery leads to raised, hypertrophic scars.
Hypertrophic scars stay within the original wound boundary, while keloids extend beyond it.
Yes, they may fade and soften over time, typically within a year, unlike keloids which may continue to grow.
They can develop anywhere but are common in high-motion areas like joints or where the skin was initially under tension.
Steroid injections can help in reducing inflammation and flattening the scar, though multiple treatments may be required.
Laser therapy can help in reducing redness and improving skin texture, making the scar less noticeable.
They can be slightly itchy or painful initially, but this usually improves as the scar matures.
Applying silicone sheets or gel, and pressure therapy, during wound healing can help in prevention.
In severe cases, especially near joints, they can restrict movement, though not as significantly as keloids or contracture scars.
Yes, though there’s a risk of scar recurrence or worsening, hence combining surgery with other treatments is often advised.

These scars start off as slightly raised scars but flatten out eventually. Flat scars are often pink or red initially and later turn darker. Flat scars are relatively easy to treat with procedures designed for resurfacing the skin.
In case of hyperpigmentation that accompanies flat scars, treatments that work on controlling melanin formation like Q switched lasers can be effective to reduce pigmentation.
The initial redness or pink color is due to blood vessels in the healing area; they darken over time due to melanin production.
Skin resurfacing removes the top layers of the scar, promoting new skin growth that’s smoother and more even-toned.
They can be long-lasting, but treatments like lasers or dermabrasion can significantly improve their appearance.
Generally, flat scars do not cause discomfort, unlike raised or contracture scars that might itch or restrict movement.
They are effective in targeting melanin and reducing pigmentation, making the scar less noticeable.
Treatments include chemical peels, microdermabrasion, and topical creams containing silicone or hydroquinone.
It’s uncommon, but possible, especially without proper wound care or if there’s an infection during the healing process.
While treatments can help, flat scars may fade over time without intervention; professional advice can provide the best course of action.
Yes, applying sunscreen prevents further darkening of the scar caused by sun exposure, promoting better healing.
Home remedies like applying vitamin E, aloe vera, or honey might help, but their effectiveness is less compared to medical treatments.


MD, DNB - Dermatology & Venereology
Scars are one of the toughest dermatological features to treat. Also not all scars can be treated. It can be possible that an attempted treatment can lead to worse outcomes than the original scar itself. Scar treatment requires a combination of medical knowledge and the latest developments in treatment methodologies available.
Dr. Sejal has more than 15 years of experience spread across thousands of patients. This experience coupled with the latest technology helps Dr. Sejal device safe yet effective plan for treatment of scars.
Dr. Sejal has dual degrees of MD and DNB in Dermatology and Venereology. She has worked with some of the senior most doctors in the largest government and private hospitals. She believes in a minimum intervention approach to health and believes that educating and empowering the patient is the key to good health.

At InUrSkn, we believe that all patient care must be:
– Holistic
– Personalized
– Humane
– Minimal
Dr. Sejal and her team live by the philosophy of never prescribing medications or procedures that may not be required. When addressing a concern, Dr. Sejal ensures that a detailed history and context are thoroughly understood. Medical tests are prescribed by Dr. Sejal only when she believes there is more to the concern that needs to be addressed, ensuring the patient truly benefits.
Our modern clinic is conveniently located in Powai, Mumbai, and is easily accessible from Hiranandani Gardens, Chandivali, and Vikhroli. Situated close to Dr. L H Hiranandani Hospital, the clinic is also easily reachable from Andheri East, Ghatkopar, and Kanjurmarg via the Jogeshwari–Vikhroli Link Road (JVLR) and the Andheri–Ghatkopar Link Road.
Multiple spacious procedure rooms
Full-fledged operation theatre
In-house laboratory
Latest technology
100+ Skin, Hair & Body Procedures offered
Frequent disinfection of all clinic spaces with UVC light and WHO-approved chemicals
Large waiting and treatment areas to ensure social distancing
Regular health checks for all patients and staff
Safer than salons, chain-clinics & hospitals
PPEs for patients and staff
Personal attention from Dr. Sejal Saheta (MD, DNB) - with 15+ years of experience
CIDESCO-certified aestheticians with minimum 3 years work experience
500+ Positive Reviews on Practo and Google
5000+ Patients treated last year alone
8000+ Procedures completed
| Prices | ||
|---|---|---|
| Procedure | ||
| In Clinic Consultation with Dr. Sejal | ||
| In Clinic Consultation with Dr. Sejal | ₹1200 | |
| Online Consultation with Dr. Sejal | ||
| Online Consultation with Dr. Sejal | ₹1000 | |
Pricing (Inclusive of taxes)


Factors include the size and depth of the wound, the person’s age, genes, and overall health, and the type of wound healing received.
Their effectiveness can vary, and while some may help to soften and reduce the appearance of scars, they are unlikely to remove scars.
A keloid is a type of scar that grows excessively beyond the boundaries of the original wound.
Laser treatment can remove the top layers of skin, promote collagen production, and improve scar texture and appearance.
While it’s not always possible to prevent scars, keeping wounds clean, avoiding irritation, and following a healthcare provider’s advice can help.
Itching can be a part of the healing process, but persistent itching should be evaluated by a healthcare provider.
Rarely, scars may lead to complications like restricted movement, especially in cases of contracture scars.
Scars form as a part of the body’s natural healing process following an injury, infection, surgery, or inflammation of the skin.
Complete removal can be challenging, but treatments can significantly reduce the appearance. Common treatments include laser therapy, surgical revision, and dermabrasion.
Scar color can vary based on an individual’s skin type, the type and location of the injury, and the healing process. Darker scars may result from hyperpigmentation.
Scars may lighten and become less noticeable over time, often over the course of several months to years, depending on the scar type and individual healing factors.
A balanced diet rich in protein, Vitamin C, and zinc can support wound healing and potentially improve scar appearance.
Smoking can impair wound healing, lead to worse scarring, and increase the risk of infection and complications.
Moderate exercise can promote blood circulation and healing, but intense or improper exercise can exacerbate scars, especially fresh surgical scars.
A normal scar typically fades over time while problematic scars like keloids or hypertrophic scars may grow or become painful/itchy. Consulting a professional is advisable.
Yes, visible or disfiguring scars can lead to self-consciousness, anxiety, or depression. Seeking psychological support can be beneficial.
Ideally one should approach dermatologist as soon as the injury starts healing and the scars start healing. Scars in their immature pinkish state are much easier to treat than mature scars.



Ready to book an appointment?
BOOK

Want to talk about your needs ?
MAKE AN enquiry
