






InUrSkn is more than just a skin a hair and body clinic. It is Dr. Sejal's promise of providing minimal intervention patient care which is holistic, personalized and humane.













Vitiligo is an autoimmune disorder, where the immune system targets melanocytes in the skin, halting melanin production and causing white patches. Often beginning between ages 30-50, its course is unpredictable, with possible rapid progression or regression of lesions. Occurring globally across all ethnicities, its triggers include stress and skin trauma. Treatment strategies range from camouflage, melanin regeneration through light therapies to pigment removal for severe cases, although it’s a non-contagious, incurable condition requiring medical intervention for management.
Read More
Pityriasis Alba (P Alba) is a prevalent skin disorder, characterized initially by red scaly patches which, upon resolution, leave hypopigmented areas. Predominantly affecting younger children, especially on their face and arms, it’s often linked to atopic dermatitis. While its exact cause remains unclear, the discolouration tends to self-resolve over time. Treatment, often symptomatic, employs topical medications for inflammation and itching, and in persistent hypopigmentation cases, excimer laser or other UV devices might be utilized to stimulate melanin production.
Read More
Pityriasis Versicolor (P Versicolor) is a fungal infection manifesting as varied colored patches primarily on the chest, back, and face, often in individuals prone to heavy sweating or those with hygiene challenges. Typically appearing in seborrheic areas like the scalp, the condition arises from an overgrowth of certain fungi impairing melanocytes, leading to hypo-pigmentation. While the patches may be white, reddish, or brownish, the disorder is manageable with antifungal shampoos or creams, and generally the discoloration self-resolves over time.
Read More
Idiopathic Guttate Hypomelanosis (IGH) is a harmless skin condition displaying as scattered hypopigmented macules or white spots, largely due to aging and prolonged sun exposure. Typically measuring 1-3 mm in diameter, these spots predominantly appear on the arms, legs, back, and face. Though its exact cause is undetermined (idiopathic), preventative measures like diligent sunscreen application and a healthy skincare routine are recommended. Treatment options include topical medications and skin rejuvenation techniques.
Read More

Not every white spot and mark is the same. While some of these may be a cause for concern, others may be absolutely benign and be nothing more than an aesthetic concern. Hence treatment of such skin ailments requires a dermatologist who is trained to differentiate between the conditions and identify treatments that work best.
Dr. Sejal’s rich experience spread over 15 years and thousands of patients puts you in safe hands. Dr. Sejal truly believes in holistic treatments that work towards eliminating the root causes rather than the symptoms.
Dr. Sejal’s approach involves not only diagnosing and treating the condition in question but also educating the patients about the causes and precautionary measures for their specific condition.

It is an autoimmune condition where body’s immune system attacks the melanocytes in the skin which are the cells responsible for producing melanin. Melanin is what provides colour to our skin. Destruction of melanocytes ensure that melanin production is stopped in the area in question and the skin turns ‘white’. Vitiligo is not a contagious disease. It can occur at any age, but is commonly seen between 30- 50 years of age. It presents as well defined white or discoloured patches on any part of the body commonly seen on hands, legs and face.
Vitiligo can be localized (restricted to few areas of the body)
Generalised( most of the areas are involved)
Universal(entire body is involved)
Hair can also get affected and become white.
Also unfortunately the course of this condition is unpredictable and hence there can be a rapid increase or decrease in vitiligo lesions.
While the exact cause of vitiligo is unknown, it is known to be hereditary. Also Vitiligo is an autoimmune disease, that is it is your body’s own immune system which malfunctions and attacks healthy cells of the body.
Vitiligo can be triggered by Stress and by any trauma to the skin. It is also known to become dominant after the body has undergone substantial stress like undergoing surgeries. Lastly Vitiligo is known to be seen in association with other conditions like diabetes, thyroid disorders and other autoimmune diseases.
As vitiligo does not have known causes besides it being hereditary, there are very few things that can be done to prevent its flare up. One of the most effective things Dr. Sejal prescribes is ensuring that one does not undertake undue stress. Any strategy that works to help a person destress from exercise to meditation to simply watching television works.
Also there are poor associations between dietary intake and other factors like environmental exposure and vitiligo and hence controlling these aspects also does not help much.
There are largely three strategies followed for vitiligo patients:
1. Camouflage
This is suitable for mild and localized cases in which small depigmented patches appear on visible areas of the body. In this case these areas are covered with temporary or semi-permanent makeup pigment to blend with the surrounding area. Treatments like microblading are suitable for covering such spots for a long lasting pigment colouration.
2. Regaining Natural Melanin
This is also suitable for mild and localized cases for repigmenting the areas in question. This uses mechanisms like excimer laser and other UV devices to stimulate melanin generation in the affected area.
3. Removing pigment from other areas
For widespread and severe cases, this may be a workable strategy where the areas with pigment are treated with topical medications to remove the pigment in those areas to achieve an even skin colour across the affected area. This strategy has to be considered with due seriousness before proceeding with the same and the treating dermatologist has to be very careful.
No, vitiligo is not contagious and there’s no need to avoid contact with affected individuals.
Yes, vitiligo affects individuals of all ethnicities and races. It may be more noticeable on darker skin, but it occurs equally.
No, vitiligo is an autoimmune condition unrelated to dietary or lifestyle choices.
No, untreated vitiligo may progress. It’s advisable to consult a dermatologist for treatment options as soon as it’s diagnosed.
Yes, treatments like topical and oral medications, as well as light therapies that stimulate melanin production, can help manage vitiligo.
Sun exposure does not typically affect vitiligo, but protecting the skin from sunburn and excessive sun exposure is advisable. Other environmental conditions generally do not affect vitiligo.
No, vitiligo and skin cancer are unrelated conditions, although individuals with vitiligo can develop skin cancer like anyone else.
No known natural or herbal remedies have been proven effective for vitiligo. It’s advisable to consult a dermatologist for treatment.

P alba stand for Pityriasis alba, which is a common skin condition in which first there is appearance of red scaly patches. When these patches resolve they leave behind areas of hypopigmentation or lighter colour.
The cause for P alba is not known. Some research states that it is a manifestation of another common condition called atopic dermatitis.
The original lesions of P alba may be red, pink or skin coloured and generally observed on face and arms. Also typically many lesions are seen together.
P alba is also more observed in younger children.
The hypopigmentation or discolouration is not permanent and often resolves automatically over a period of time.
As the reasons for this condition are largely unknown there is not much that can be done to prevent this condition.
P alba is largely resolved using topical medications. Most of the treatment is symptomatic in nature with certain low potency corticosteroid being prescribed by the treating dermatologist to resolve inflammation. Some other topical medications may be prescribed to reduce itching and redness.
If the hypopigmentation post initial lesions persists then it can be treated with excimer laser of other UV energy devices to stimulate melanin formation.
Diagnosis is primarily clinical, based on the appearance of the skin. A dermatologist may perform a physical examination or skin biopsy if necessary.
Yes, it’s more common in children, although it can occur at any age.
No, the hypopigmentation usually resolves over time without leaving permanent marks.
Prevention is challenging due to the unknown cause, although managing atopic dermatitis can potentially minimize its occurrence.
The exact triggers are unknown, but it’s often associated with atopic dermatitis.
While the condition often resolves on its own, medical treatment can manage symptoms and expedite the fading of hypopigmentation.
There isn’t a known cure, but moisturizing the skin can help alleviate dryness and improve appearance. However, consult a dermatologist before trying any remedy.
Sun exposure can make the hypopigmentation more noticeable, but it doesn’t cause the condition. Using sunscreen may help in reducing contrast.
It’s often associated with atopic dermatitis but not conclusively linked to other skin conditions.
It can recur, especially in individuals with a history of atopic dermatitis or other dermatological conditions.
Not at all. It is an idiopathic condition which cannot be transmitted by any mechanism.
Yes absolutely. Although the treatments are targeted at the symptoms. P alba resolves completely in almost 100% of the cases.
P alba is not affected in any manner for either environmental factors or by lifestyle choices.
Generally P alba is associated to atopic dermatitis. Besides this there are no other associated conditions.

Pityriasis Versicolor or P Versicolor is fungal infection seen in the form of multiple whitish patches and spots mainly on chest, back and face. It is also sometimes called tinea versicolor.
P versicolor normally affects people who may sweat heavily or may have issues with maintaining hygiene. As this condition is ideal for fungal growth on the skin. This condition is infectious even if it has low rate of spread.
While it is normally described as white patches, it can also appear as reddish or brownish patches.
It usually appears on the seborrhoeic areas of the body namely scalp, face, chest and back. It occurs when a certain fungus undergoes rapid growth on our skin which impairs the function of melanocytes causing hypo-pigmentation.
Since the primary causative factor is fungal growth. It follows that flare ups of such conditions can be prevented by maintaining better hygiene including but no limited to regular bathing and keeping the areas in concern dry and devoid of excess moisture.
The most common types of treatment for P versicolor remain in the form of anti fungal shampoo for scalp and gel or cream for skin. The discoloured patches left behind generally do not need any intervention and resolves by itself.
Diagnosis is usually through clinical examination; a dermatologist may inspect the skin and perform a Wood’s lamp examination or skin scraping for microscopic analysis.
Hot, humid environments and excessive sweating can create favorable conditions for fungal overgrowth. Maintaining good hygiene can help in reducing the risk.
It can recur especially in warm, humid climates or in individuals with a predisposition to excessive sweating.
Regular bathing, keeping the skin dry, and avoiding oily products can help prevent fungal overgrowth. In addition, wearing loose, breathable clothing may be beneficial.
Treatment duration can vary, but usually, significant improvement is seen within a month of adhering to the treatment protocol.
No, the discoloration is temporary and usually resolves over time once the fungal infection is treated.
It can cause mild itching, but it’s usually not painful or significantly uncomfortable.
Over-the-counter antifungal creams can be effective, but it’s advisable to consult with a dermatologist for a proper diagnosis and treatment plan.
It can affect individuals of all ages but is more common in adolescents and young adults due to hormonal changes affecting the skin.
Yes, it can spread to other parts of the body, particularly seborrheic areas like the scalp, face, chest, and back.
Being a fungal infection, it can be infectious. But it does not spread easily.
Yes. As it is a fungal infection, anti-fungal creams and shampoos are very effective on skin and scalp respectively. It resolves mostly within a month of following the correct treatment protocol.
Yes. Hot and humid environment is suitable for spread of P versicolor. In dry and cool weather P versicolor clears out. Also personal hygiene plays a big role in reducing the incidence of such conditions which generally takes hold in individuals who perspire too much and maintain poor hygiene.
The name P versicolor reflects that fact that it may have different presentations on different individuals. Some lesions are white, while others may be red or brown.
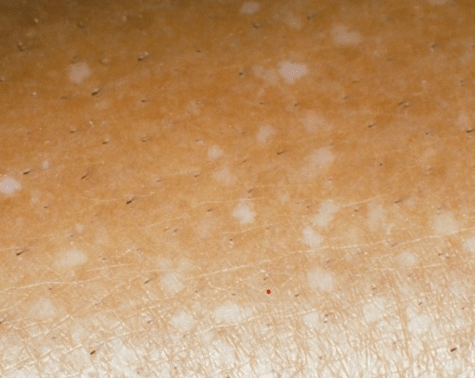
Idiopathic Guttate Hypomelanosis (IGH) is a benign and asymptomatic skin manifestation characterized as diffuse hypopigmented macules, or white spots. The size of the lesions varies from 1-10mm, but are most commonly 1-3 mm in diameter.
It is mainly caused for ageing and sun exposure over a long period of time. These lesions are generally visible on the arms, legs, back and face.
As the name of the condition suggest that it is largely idiopathic (that is there is no known reasons for this to occur) However there is a co-relation established between ageing and sun exposure and this condition.
Because of the known relation between sun exposure and this condition, patients are advised to use sunscreen religiously to prevent more spots from occurring. Also maintaining a healthy daily skin care routine helps.
This condition can largely be solved with topical medications and may benefit from certain skin rejuvenation techniques.
It is possible to reduce the occurrence of IGH lesions by means of using sunscreens and protecting yourself from the sun. However this is not foolproof.
Yes. The lesions can be treated with topical applications. Also it is interesting to note that IGH is largely benign in nature.
It is mainly ageing and cumulative sun exposure that are the reasons for IGH.
Diagnosis is often clinical, based on the appearance of the lesions. A dermatologist may perform a skin examination to identify the characteristic white spots.
No, IGH is not contagious as it is a benign skin condition associated with aging and sun exposure.
IGH is asymptomatic, meaning it does not cause any physical discomfort, itchiness, or pain.
No, IGH does not lead to other skin complications as it is a benign condition.
Individuals with prolonged sun exposure and older age groups are more prone to IGH.
Topical steroids or calcineurin inhibitors, and compounds that promote pigmentation can be used for treating IGH. It’s advisable to consult with a dermatologist for personalized treatment.
Yes, laser treatments like fractional CO2 laser can help in improving the appearance of IGH lesions.
Regular use of sunscreen and minimizing sun exposure can help in preventing IGH from worsening.
IGH spots do not generally disappear on their own, but their appearance can be improved with treatment.
Aging may lead to a reduction in melanin production, making the skin more susceptible to the effects of sun exposure which can trigger IGH.


MD, DNB - Dermatology & Venereology
Dr. Sejal has dual degrees of MD and DNB in Dermatology and Venereology. She has worked with some of the senior most doctors in the largest government and private hospitals for more than 15 years. Over these years at InUrSKn, she has treated thousands of patients for a variety of conditions and needs across dermatology, venereology, cosmetology and trichology domains.
Dr. Sejal believes in a minimum intervention approach to health and believes that educating and empowering the patient is the key to good health.
Every patient at InUrSkn is seen personally by Dr. Sejal without any time limit, where she discusses the patient’s concern in detail along with understanding the history of their health and carrying out a personal examination.

At InUrSkn we belive that all patient care must be
– Holistic
– Personalized
– Humane
– Minimal
That is Dr. Sejal and Team live by the philospohy to never prescribe medications or procedures that may not be required and while approaching a concern Dr. Sejal ensures that a detailed history and context is understood by her. Medical tests are prescribed by Dr. Sejal when she believes that there is more to the concern which needs to be addressed and only then the patient can truly benefit.
Multiple spacious procedure rooms
Full-fledged operation theatre
In-house laboratory
Latest technology
100+ Skin, Hair & Body Procedures offered
Frequent disinfection of all clinic spaces with UVC light and WHO-approved chemicals
Large waiting and treatment areas to ensure social distancing
Regular health checks for all patients and staff
Safer than salons, chain-clinics & hospitals
PPEs for patients and staff
Personal attention from Dr. Sejal Saheta (MD, DNB) - with 15+ years of experience
CIDESCO-certified aestheticians with minimum 3 years work experience
500+ Positive Reviews on Practo and Google
5000+ Patients treated last year alone
8000+ Procedures completed
| Prices | ||
|---|---|---|
| Procedure | ||
| In Clinic Consultation with Dr. Sejal | ||
| In Clinic Consultation with Dr. Sejal | ₹1100 | |
| Online Consultation with Dr. Sejal | ||
| Online Consultation with Dr. Sejal | ₹900 | |
| Microbladed Brows | ||
| Microbladed Brows | ₹30000 | |
| Microblading of Lips | ||
| Microblading of Lips | ₹20000 | |
| Microblading of Spots on skin and scalp | ||
| Microblading of Spots on skin and scalp | ₹10000 to 40000 | |
Pricing (Inclusive of taxes)


Common causes include fungal infections, vitiligo, hypopigmentation disorders, or skin reactions to inflammation or irritation.
While often benign, white spots or patches should be evaluated by a healthcare professional to determine the cause and appropriate treatment, if necessary.
Yes, prolonged sun exposure can trigger or worsen conditions leading to white spots or patches on the skin.
Prevention may be possible by avoiding triggers such as excessive sun exposure, maintaining good hygiene to prevent infections, and following a healthy skincare routine.
Over-the-counter antifungal creams or lotions can treat some causes of white spots, though it’s advisable to consult with a healthcare professional for an accurate diagnosis and treatment plan.
While not commonly, certain nutritional deficiencies can result in skin discoloration. It’s advisable to consult with a healthcare professional for a personalized assessment.
The duration varies widely depending on the cause; some conditions resolve in weeks, while others may take months or longer. Treatment may expedite resolution.
Some conditions causing white spots or patches may itch or cause discomfort, while others are asymptomatic.
Recurrence is possible depending on the underlying cause. Following treatment and prevention guidelines can reduce the likelihood of recurrence.
Cosmetic products like concealers or foundation can temporarily cover discoloration, though they do not treat the underlying condition.
Yes, some conditions are more common in certain age groups, and skin type or genetic factors may also play a role.
Stress might exacerbate some skin conditions leading to discoloration, although it’s not a common direct cause.
A balanced diet supports overall skin health, but specific dietary changes should be discussed with a healthcare professional.
Hormonal changes can affect skin conditions, potentially leading to discoloration in some individuals.
Exfoliation may not be advisable for all skin discoloration conditions and could irritate the skin further. It’s best to consult with a healthcare professional.

It is sometimes the small things in life that make the biggest difference. Dr. Sejal firmly believes in the concept of continuous imporvement be it in her practice or a patient's health.
Here you will find quick tips on all things related to skin, hair and body.

Ready to book an appointment?
BOOK

Want to talk about your needs ?
MAKE AN enquiry
